A new preclinical study suggests that a compound in cannabis may serve as a potential treatment for patients with Alzheimer’s disease.
A recent study, conducted by neuroscientists at the University of South Florida, shows that extremely low levels of the compound in cannabis, known as delta-9-tetrahydrocannabinol, or THC, may slow or halt progression of the disease. Findings from the experiments, using a cellular model of Alzheimer’s disease, were reported online in the Journal of Alzheimer’s Disease.
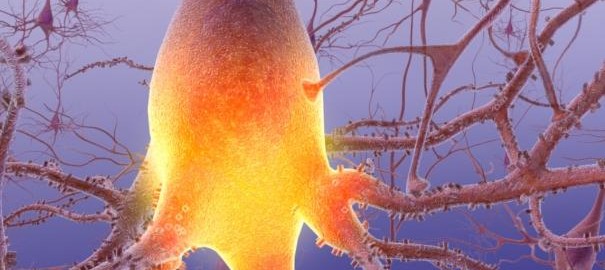
Researchers from the USF Health Byrd Alzheimer’s Institute showed that extremely low doses of THC reduce the production of amyloid beta, found in a soluble form in most aging brains, and prevent abnormal accumulation of this protein, a process considered one of the pathological hallmarks evident early in the disease. Additionally, the low concentrations of THC selectively enhanced mitochondrial function, which is needed to help supply energy, transmit signals, and maintain a healthy brain.
“THC is known to be a potent antioxidant with neuroprotective properties, but this is the first report that the compound directly affects Alzheimer’s pathology by decreasing amyloid beta levels, inhibiting its aggregation, and enhancing mitochondrial function,” said study lead author Chuanhai Cao, PhD and a neuroscientist at the Byrd Alzheimer’s Institute and the USF College of Pharmacy. “Decreased levels of amyloid beta means less aggregation, which may protect against the progression of Alzheimer’s disease. Since THC is a natural and relatively safe amyloid inhibitor, THC or its analogs may help us develop an effective treatment in the future.”
According to the researchers, at the low doses of THC studied, the therapeutic benefits appear greater than the risks of toxicity and memory impairment associated with THC.
“While we are still far from a consensus, this study indicates that THC and THC-related compounds may be of therapeutic value in Alzheimer’s disease,” said study co-author Neel Nabar, MD/PhD candidate. “Are we advocating that people use illicit drugs to prevent the disease? No. It’s important to keep in mind that just because a drug may be effective doesn’t mean it can be safely used by anyone. However, these findings may lead to the development of related compounds that are safe, legal, and useful in the treatment of Alzheimer’s disease.”
The body has a system of cannabinoid receptors that interacts with naturally-occurring cannabinoid molecules. These molecules function similarly to the THC isolated from the cannabis plant. Dr. Cao’s laboratory is currently investigating the effects of a drug cocktail consisting of THC, caffeine and other natural compounds in a cellular model of Alzheimer’s disease. The investigators will advance to a genetically-engineered mouse model of Alzheimer’s shortly.
“The dose and target population are critically important for any drug, so careful monitoring and control of drug levels in the blood and system are very important for therapeutic use, especially for a compound such as THC,” Dr. Cao stated.
According to the Centers for Disease Control and Prevention (CDC), as many as 5 million Americans suffer from Alzheimer’s disease, with numbers projected to reach 14 million by 2050.
Source: Chuanhai Cao, Yaqiong Li, Hui Liu, Ge Bai, Jonathan May, Xiaoyang Lin, Kyle Sutherland, Neel Nabar and Jianfeng Cai; “The Potential Therapeutic Effects of THC on Alzheimer’s Disease,” Journal of Alzheimer’s Disease, DOI: 10.3233/JAD-140093.
Last updated: 8/28/14; 10:45am EST